What is relapsing multiple sclerosis (MS)?
Understanding the details can help
Relapsing multiple sclerosis (MS) is a progressive disease that damages the central nervous system (CNS). Although there is no cure for the disease, many relapsing MS treatment options are available that can help slow its progression.
affects the body
Relapsing MS is thought to be an autoimmune disease, which means that instead of defending the body against harmful invaders (such as viruses or bacteria), the immune system attacks the CNS.
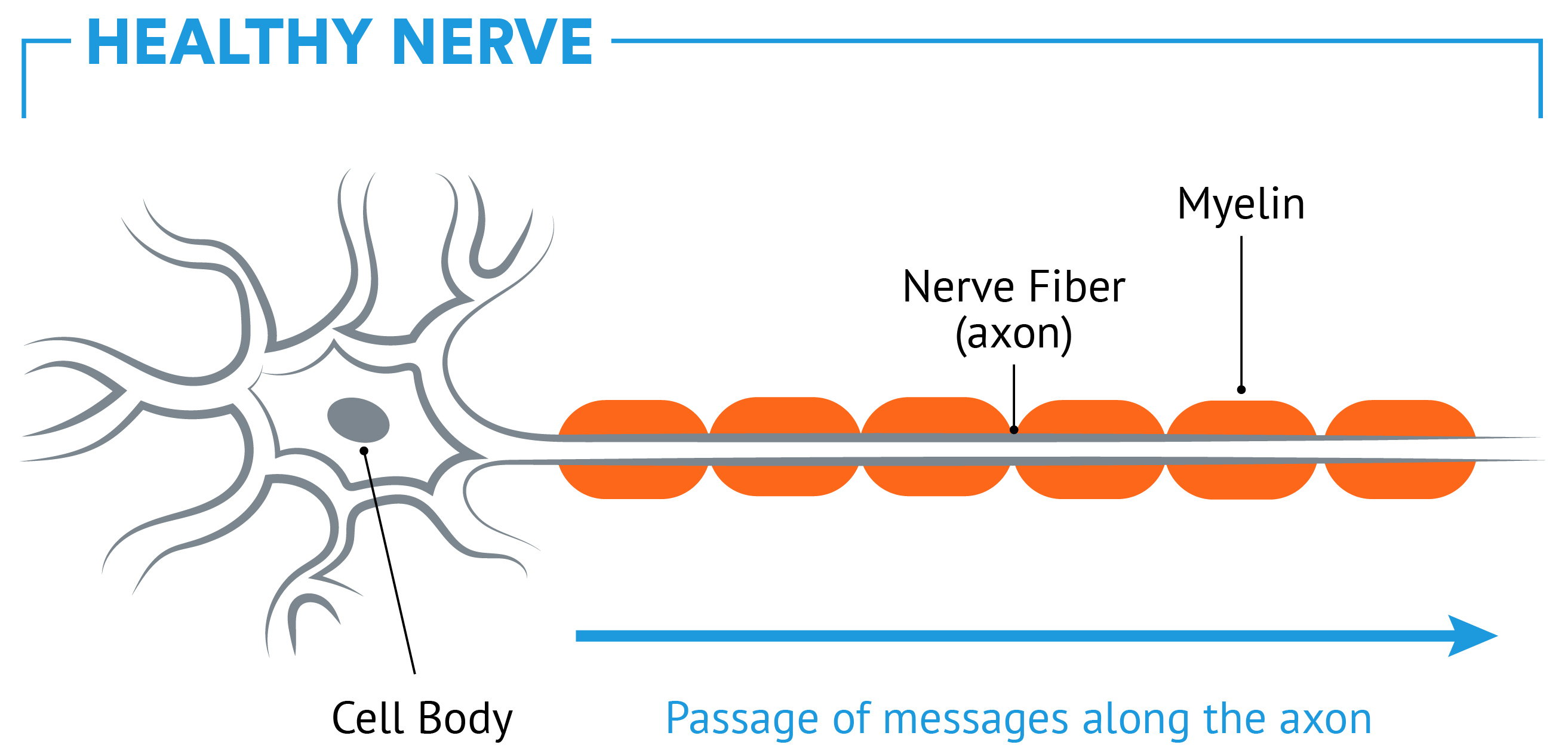
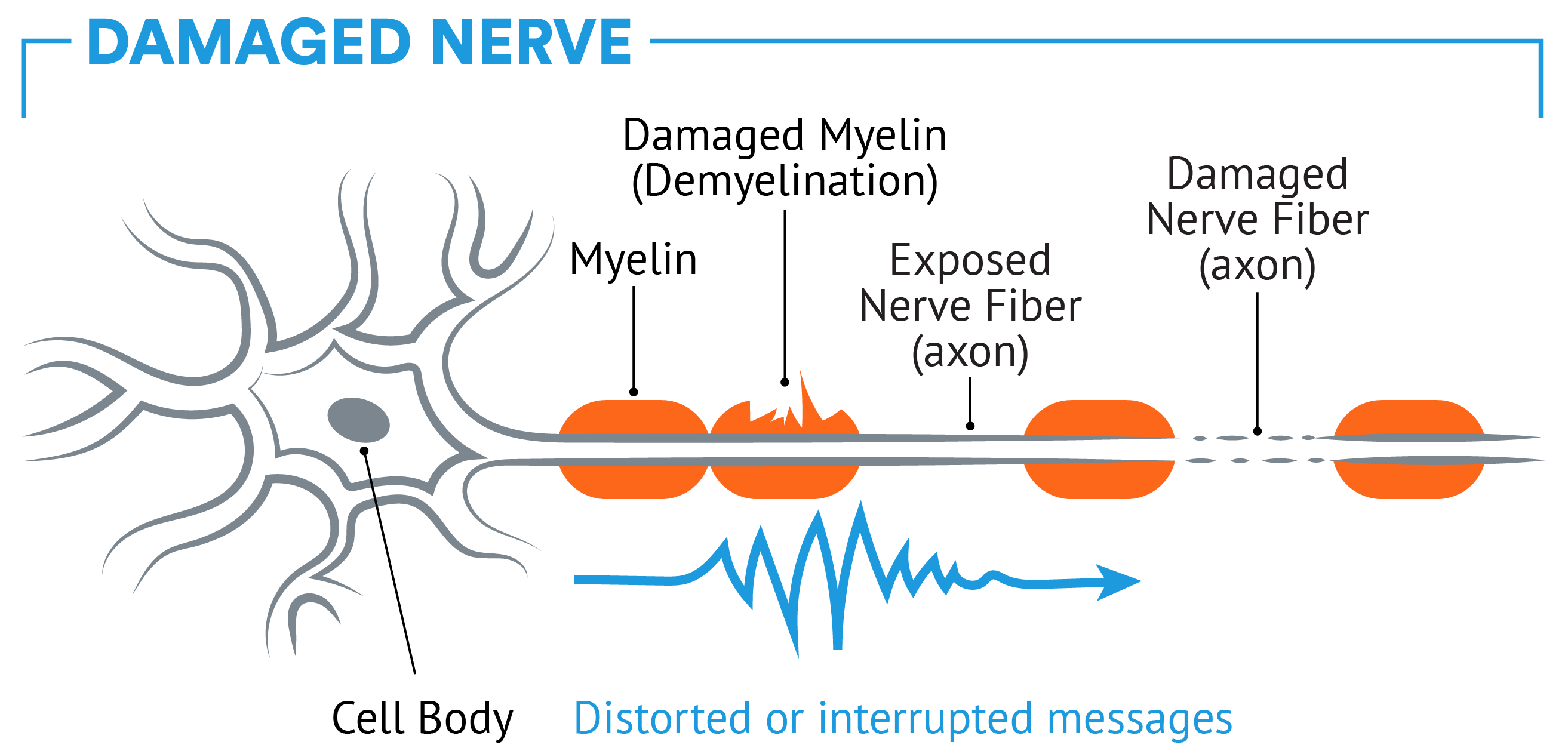
The CNS contains nerve cells called neurons. Each neuron has a covering that functions like a rubber coating around an electrical wire. This coating, known as the myelin sheath, protects the nerve inside. The myelin also helps neurons send electrical signals to and from the brain, telling the body what to do.
In people with MS, immune cells enter the CNS and attack the myelin sheath. This is thought to interfere with the ability of neurons to send signals between the brain and the body. When your brain cannot communicate with the nerves and muscles the way it’s supposed to, MS symptoms can occur. Reducing these symptoms is a key goal when determining how to treat MS.
Nobody knows exactly what causes MS, but research is being conducted to investigate some possible causes such as:
- Environmental elements
- Infectious agents (such as bacteria or a virus)
- Genetic predisposition (a family history of MS)
- Ethnicity: although anyone can get relapsing MS, a large percentage of MS patients are of Northern European descent
Relapsing MS is about 2-3 times more common in women than in men. An MS diagnosis generally occurs between 20 and 50 years of age, but it can also happen when you’re younger or older.
As your disease progresses, existing MS symptoms may worsen, or new symptoms may appear during a relapse. If you have any questions about relapsing MS symptoms, or how to treat MS, the best source of information is your healthcare team.
Some of the common symptoms of relapsing MS include:
Note that there are currently no disease-modifying therapies (DMTs), including TYSABRI, indicated to treat these symptoms:
- Bladder and bowel problems
- Difficulties with attention, learning, and memory
- Mood changes
- Fatigue
- Muscle rigidity or stiffness
- Weakness or poor coordination and dizziness
- Numbness and tingling
- Pain in arms and legs
- Vision problems
To learn more about the symptoms of relapsing MS, talk with your healthcare provider.
Relapses, also known as MS flare-ups or exacerbations, are new symptoms not brought on by fever, heat, or infection, or a worsening of symptoms you already have. Relapses are unpredictable. They can last from a few days to several months and some are worse than others. Even infrequent or mild relapses can cause permanent damage to the CNS and may lead to future disability. That’s why it’s important to take every relapse seriously and talk to your healthcare team right away.
lesions?
MS causes brain lesions that can be seen with magnetic resonance imaging (MRI). MRIs show recent lesion development as well as damage from older lesions. Some common types of MS-related brain lesions that can be seen with MRIs include:
- Gd+ enhanced lesions: Lesions that show active inflammation, which are detected on MRI using a dye containing the chemical element gadolinium
- Lesions: Some lesions show the long-term impact of inflammation on your brain, while others show active inflammation
The exact relationship between MRI findings and your overall health is not clear. However, MRIs are commonly used to help you and your healthcare team monitor disease activity in your body. While healthcare providers can’t say for sure if there is a link between brain lesions and the progression of disability, it is important to talk with your neurologist about each one of your MRIs because that may help with developing a plan for how to treat your MS.
It is important to remember that underlying MS activity could be damaging your CNS whether or not you are experiencing symptoms. So even if you’re feeling fine, your MS may be worsening and you might experience new symptoms later on.
Many studies have shown that permanent nerve damage can happen during relapses. These relapses may contribute to disability progression. To help slow this progression, talk with your healthcare provider about starting treatment with an FDA-approved medication as soon as you are diagnosed.
It is important to do your research about how to treat MS. Look at the ways that different treatment options are believed to work. Find out about their clinical studies, side effects, and effectiveness. Bring up specific concerns about safety and side effects with your healthcare team. Learning all you can empowers you to make a confident decision with your healthcare team.
Some different treatment options include:
- Injections
- Infusions
- Oral pills
from Biogen
TYSABRI is one of several relapsing MS treatments available from Biogen. It is indicated for the treatment of patients with relapsing forms of MS, to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease. TYSABRI is not indicated to treat the individual symptoms of relapsing MS, including those described above.
Remember that your healthcare team is always your best source of information, and you should work with your doctor to find the treatment option that is best for you.
